Introduction
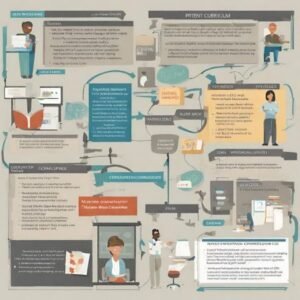
In the current scenario of medical education, a significant transformation is underway: reinventing medical teaching. The transition to a professional competency-based curriculum marks a promising advancement, preparing future physicians to meet the complex demands of contemporary clinical practice.
This article explores the essence of this evolution, highlighting how it equips healthcare professionals with the tools they need to excel in a dynamic environment.
The Demand for Change
Reinventing Medical Teaching
The transition to a competency-centered curriculum is a direct response to demands for more effective, safe, and patient-centered health care. Faced with rapid technological advances and the need for an interprofessional approach to healthcare, today's medical professionals must possess not only deep theoretical knowledge, but also robust practical skills, a solid ethical understanding, and a capacity for continuous learning. Therefore, a competency-based CV is essential to ensure that doctors are well equipped to face these challenges.
At the heart of the modern healthcare system we find a dynamism driven by rapid technological advances, emerging ethical challenges is increasingly diverse patient population. This complex and constantly evolving landscape raises a fundamental question: How can traditional medical curricula adapt to effectively prepare students for the realities of today's medical practice?
The answer to this critical question lies in the evolution toward a medical curriculum based on professional competencies. This innovative approach transcends the traditional educational paradigm, which focuses predominantly on the accumulation of theoretical knowledge. In contrast, the competency-based curriculum is dedicated to the holistic development of the medical student, emphasizing not only the acquisition of knowledge but also the enhancement of practical skills, the exercise of clinical judgment, and ethical sensitivity.
Implementing Changes
The implementation of a curriculum based on professional competencies represents a significant transformation in medical education. It requires a reassessment of values, a reconceptualization of pedagogical methods and a restructuring of assessment programs. This multifaceted process aims to align medical curricula with the contemporary needs of the healthcare system, ensuring that future doctors are well-equipped to face complex clinical challenges, make informed ethical decisions, and respond effectively to the expectations of a diverse society.
Challenges and Opportunities
The transition to a competency-based curriculum is not without its challenges. It involves overcoming institutional resistance, adapting educational resources and ensuring buy-in from all stakeholders. However, the opportunities that arise from this transformation are immense. A competency-based curriculum promotes more relevant, adaptive and responsive medical education, capable of preparing professionals to perform excellently in a rapidly changing healthcare environment.
The Role of Assessment
Assessment plays a central role in competency-based medical education. Rather than focusing exclusively on tests of theoretical knowledge, assessments in a competency-based curriculum cover a diverse range of skills and behaviors through the diverse use of assessment instruments. This includes the ability to apply knowledge in clinical settings, the effectiveness of communicating with patients and healthcare teams, and the readiness to confront ethical dilemmas. Through innovative assessment methods such as simulations, OSCEs (Objective Structured Clinical Exams) and 360-degree feedback, competency-based programs ensure comprehensive and deeply integrated medical training.
The Future of Medical Education
The future of medical education lies in the adoption of curricula based on professional skills. This approach not only prepares physicians to be skilled and compassionate professionals, but also empowers them to lead healthcare transformation. As we move forward, it is essential that medical education institutions continue to innovate, adapt and evolve, ensuring the next generation of doctors is ready to meet the demands of an ever-changing world.
The demand for change in medical education is clear and imperative. As we move toward a professional competency-based medical curriculum, we pave the way for an era of medical education that equally values knowledge, practical skills, and ethical judgment. This evolution promises to not only improve health outcomes for patients around the world, but also enrich the professional journey of future doctors, equipping them to face the challenges and opportunities of the 21st century.
What Are Professional Skills?
Professional competencies are combinations of skills, knowledge, and attitudes that enable physicians to provide high-quality care. These competencies encompass a broad range of skills, including accurate execution of clinical procedures, effective communication, application of critical and scientific reasoning, as well as a commitment to ethics and ongoing professional development. To develop such skills, a curriculum that promotes a holistic, experience-based and reflective education is necessary.
Exploring Professional Skills
In the world of medical education, the introduction of curricula based on professional skills represents a fundamental transformation. This approach not only expands the scope of medical training, but also redefines the role of doctors in contemporary society. Professional skills, in this context, go beyond the domain of traditional medical knowledge, encompassing a broader set of skills crucial for effective clinical practice.
The essence of professional skills in medicine lies in their ability to integrate knowledge, skills and attitudes in a way that empowers clinicians to respond effectively to patient needs and healthcare system challenges. This includes the ability to apply theoretical knowledge in real clinical scenarios, make informed and evidence-based decisions, and use emerging technologies ethically and responsibly.
Effective communication emerges as a key competence, highlighting the importance of meaningful interactions with patients, families and multidisciplinary teams. The ability to actively listen, convey information clearly and empathetically, and build trusting relationships is fundamental to successful patient care.
Another critical dimension of professional skills is the medical ethics and clinical judgment. Doctors regularly face complex ethical dilemmas that require a capacity for deep reflection, consideration of patients' values, and a commitment to the fundamental ethical principles of medicine.
O continuous learning is equally essential, emphasizing the need for physicians to stay up to date with advances in medical science and clinical practices. This involves a willingness to continually self-improve and adapt to new information and technologies that can improve patient care.
Competency-based practice also recognizes the importance of interprofessional collaboration. No doctor operates in isolation; The ability to work effectively within interdisciplinary teams is vital to providing comprehensive, coordinated care.
Finally, competency-based medical education challenges future physicians to develop a holistic view of health. This includes health promotion and disease prevention, as well as a commitment to public health and the well-being of the broader community.
As we explore the professional competencies needed for 21st century physicians, it becomes clear that medical education must be as dynamic and multifaceted as the field of medicine itself. The professional competency-based medical curriculum is not just a methodological shift, but a fundamental reorientation that prepares physicians to be not only healers but also leaders, innovators, and patient advocates in a rapidly changing world.
Benefits of a Competency-Driven Curriculum
1. Adaptation to the evolution of medicine
At the heart of the evolution of medical education, competency-driven curricula emerge as beacons of innovation and adaptation. This approach, which transcends the traditional accumulation of knowledge to emphasize practical skills, clinical judgment, and ethical sensitivity, prepares future physicians to deftly navigate the dynamic healthcare environment. Adapting to the evolution of medicine It is, therefore, more than a necessity; it is an educational imperative.
A preparation for self-directed and continuous learning is one of the pillars of this model. In today's world, marked by rapid technological advances and increasing complexities in healthcare, the ability to continually learn and adapt is critical. Professional competency-oriented curricula not only recognize this reality, but actively prepare students for it.
A integration of knowledge, skills and attitudes forms the basis on which competency-based curricula are built. This holistic approach not only enables students to apply theory to practice, but also to navigate the ethical and communicational challenges of the medical profession with insight and empathy.
Fostering clinical judgment and ethical sensitivity — In a world where ethical dilemmas and complex decisions are everyday, training doctors with a firm moral compass and keen clinical judgment is crucial. Competency-based curricula pay special attention to developing these qualities, preparing physicians to make informed, patient-centered decisions.
A emphasis on continuous learning reflects the understanding that medicine is a profession of constant evolution. By promoting self-improvement and constant updating, competency-based curricula ensure that doctors remain at the forefront of advances in their field.
Promoting interprofessional collaboration is another significant benefit. When treating patients, doctors often collaborate with professionals from various disciplines. Competency-oriented curricula prepare students to work effectively in multidisciplinary teams, recognizing the importance of each member in patient care.
To the address the needs of a diverse patient population, these curricula prepare future doctors to provide care that is sensitive to patients' diverse cultures, beliefs, and social contexts. This respect for diversity and inclusion is vital in contemporary medical practice.
2. Patient-Centered Curriculum
The implementation of a Competency-Based Curriculum in medical training provides a series of significant benefits, both for students and for the healthcare system as a whole. This education model focuses on the development of skills, knowledge and attitudes essential for medical practice, aligning the educational process with the real needs of patients and the healthcare system.
Patient-Centered, the competency-based curriculum promotes a more humanized and effective approach to care. By emphasizing the importance of understanding and meeting patients' holistic needs, future physicians are trained to establish stronger trusting relationships, which is critical to improving health outcomes. This patient focus ensures that medical care is not only technically competent, but also empathetic and tailored to each patient's individual needs.
The competency approach facilitates a active, student-centered learning, encouraging the development of critical thinking, problem solving and continuous learning. This prepares medical students to adapt to rapid changes in the healthcare field and changing patient needs, ensuring up-to-date and relevant medical training.
Furthermore, the competency-based curriculum promotes better integration between theory and practice, offering students opportunities to apply theoretical knowledge in real clinical scenarios. This not only reinforces learning, but also improves students' preparation for the challenges of medical practice.
Continuous formative assessment is another central pillar of this educational model. It allows the constant monitoring of student progress, identifying areas of strength and need for improvement. This ensures more personalized and effective medical training, adjusted to the learning needs of each student.
Implementing a competency-based curriculum also has a positive impact on quality of health care. By preparing more qualified and adaptable professionals, this model contributes to raising standards of medical practice, which translates into better patient care and greater efficiency in the healthcare system.
Adopting a competency-based curriculum in medical training therefore represents a significant step towards a more efficient, equitable and patient-centered healthcare system. By preparing medical professionals who are not only technically proficient but also able to meet the complex needs of patients with empathy and effectiveness, we are paving the way for a brighter future in healthcare.
3. Comprehensive Assessment
The transition to a Competency-Based Curriculum in medical education brings a profound transformation not only in the syllabus, but also in the way students' progress is assessed. Gone are the days when academic success was measured solely by standardized tests and final exams. At the heart of this change lies the principle of Comprehensive Assessment, a critical component that provides a holistic view of student development, supporting more effective educational interventions and ensuring a higher standard of clinical practice.
Comprehensive assessment transcends the simple measurement of theoretical knowledge. It emphasizes a detailed analysis of clinical skills, communication skills, critical reasoning, and ethical proficiency. This means that in addition to knowing 'what', it is equally important to evaluate 'how' and 'why' future doctors apply their knowledge in practice. This multifaceted approach ensures that students are not only absorbing information, but also developing the essential skills for effective and humanized medical practice.
The implementation of evaluation methods such as Objective Structured Clinical Examination (OSCE), 360-degree assessments, Mini-CEX, and reflective portfolios, among others, allow educators to measure student performance in a variety of clinical and interprofessional contexts. These assessment tools provide accurate feedback on students' ability to integrate and apply knowledge in real-world scenarios, facilitating more targeted and personalized learning.
Furthermore, comprehensive assessment favors the development of individualized learning plans, allowing students to identify and work on their areas of weakness. This not only improves academic and clinical performance, but also promotes a culture of self-assessment and continuous learning, which are fundamental to lifelong medical practice.
This assessment model also has a significant impact on quality of healthcare provided. By ensuring that all graduates achieve a high standard of clinical and professional competence, medical education programs contribute to the training of professionals capable of providing safe, effective and patient-centered care.
Additionally, the comprehensive assessment encourages collaboration and effective communication within multidisciplinary health teams. By assessing communication and teamwork skills, competency-driven curricula prepare students for the collaborative reality of modern medical practice.
By understanding the benefits of comprehensive assessment in a competency-based curriculum, it is essential to also explore the strategies and challenges for implementing such assessment methods. In the following section, we will discuss innovative approaches and obstacles faced by institutions when adopting assessment systems that support the continued development of medical students' professional competencies.

Implementing the Competency-Based Curriculum
Implementing a competency-based medical curriculum involves clearly defining the skills that graduates must acquire and structuring learning experiences that foster the development of these skills. This includes interactive teaching methods such as problem-based learning (PBL) and clinical simulations, as well as supervised internships and research projects. Formative and summative assessment plays a crucial role, providing ongoing feedback and identifying areas for improvement
1. Definition of Competencies
The implementation of a competency-based curriculum (CBC) in medical education represents a paradigmatic shift, focusing on the acquisition and demonstration of essential skills required for medical practice. This section explores the critical steps for effective CBC implementation, with a focus on medical education.
Definition of Competencies: The first step involves clearly identifying the skills that trainees must demonstrate upon completing the course. These competencies are derived from social needs, professional standards and ethical expectations, ensuring that future doctors are prepared to meet the demands of society. O CanMEDS offers a comprehensive model, outlining key competencies such as effective communication, critical thinking, and interprofessional collaboration. Just like the DCN of Medicine present the Brazilian model for defining the three main areas of competences for the medical course.
Curriculum Development: After defining the competencies, the next step is to develop the curriculum that will support students in acquiring these skills. This includes creating interactive teaching modules, problem-based learning (PBL) experiences, and simulations that reflect real-life scenarios. The integration of modern educational technologies, such as virtual reality and e-learning, can enrich this process.
Active Teaching-Learning Methodologies: The adoption of active teaching methodologies is essential at CBC. Strategies such as Problem-Based Learning (PBL) encourage students to actively engage in their learning, developing problem-solving and critical thinking skills in realistic clinical contexts. These approaches promote learner autonomy and the practical application of theoretical knowledge.
Formative and Summative Assessment: Assessment is a crucial component of CBC, requiring methods that accurately measure student progress toward defined competencies. Formative assessment, carried out throughout the course, allows timely adjustments to the learning process, while summative assessment, at the end of the course, validates the student's competence. Instruments like OSCE (Objective Structured Clinical Examination) and Mini-CEX (Clinical Evaluation Exercise) are effective examples of competency-based assessment.
Continuous Feedback: Feedback is vital for students’ continuous development and improvement. It should be specific, constructive and timely, allowing students to reflect on their performances and identify areas for improvement. Establishing a culture of positive and open feedback contributes to a collaborative and supportive learning environment.
Teacher Professional Development: For successful implementation of CBC, medical educators must be prepared to teach within this framework. This entails ongoing training in medical pedagogy, competency-based assessment and feedback techniques. A commitment to teacher professional development ensures that faculty are equipped to effectively facilitate competency-based learning.
The transition to a competency-based curriculum in medical education is a complex process that requires institutional commitment, adequate resources, and a cultural shift toward student-centered learning. By strategically following these steps, medical education institutions can not only meet contemporary medical training demands but also prepare highly competent and adaptable professionals. Moving on, the next section will address "Active Teaching-Learning Methods", focusing on how these practices are fundamental for the continuous development of skills in medical students.
2. Active Teaching-Learning Methods
the implementation of Active Teaching-Learning Methods is a fundamental pillar for the success of a medical curriculum based on professional skills. These methods, which include Problem-Based Learning (PBL), Project-Based Learning (PjBL), It is clinical simulations, promote a more integrated, practical medical education aligned with the real needs of the healthcare environment.
O PBL, for example, puts students face to face with real challenges that they will have to solve throughout their careers, stimulating not only clinical reasoning and decision-making, but also communication skills. team work It is Effective communication. This method is not new, having first been introduced in the late 1960s, and has since been widely adopted by medical schools around the world due to its effectiveness in preparing students for actual medical practice.
A Project-Based Learning goes further, encouraging students to develop and implement projects that can have tangible impacts on the community. This not only develops practical skills but also emphasizes the social responsability and the medical ethics, crucial components of professional skills in medicine.
Clinical simulations, another important aspect of active methods, allow students to practice procedures and make decisions in a controlled environment, reducing risk to real patients and increasing the confidence of future doctors before entering clinical practice.
Implementing these methods requires a significant change in pedagogical approach, moving from an education based primarily on the transmission of knowledge to one that is student-centered, where the self-directed learning and the critical reflection are encouraged. This requires not only curricular restructuring, but also an investment in teacher training It is infrastructure, including educational technologies that support such methods.
Furthermore, student assessment must also evolve to reflect this competency-based approach. Instead of focusing solely on traditional exams, assessment should incorporate continuous feedback, self-evaluation It is peer review, offering a more complete view of student development.
In short, the adoption of active teaching-learning methods in the competency-based medical curriculum is essential to prepare healthcare professionals capable of facing the challenges of modern medicine. This educational transformation not only improves students' clinical skills and readiness for medical practice, but also promotes values such as empathy, ethic It is social responsability, essential for medical practice.
3. Diverse Assessments
Implementing the Competency-Based Curriculum in the field of medicine requires a multifaceted approach, particularly when it comes to Diverse Assessments. This crucial aspect ensures a holistic assessment of students' competencies, going beyond mere theoretical knowledge to include practical skills, clinical reasoning, professional ethics and communication skills.
The transition to a competency-based assessment model it means integrating a variety of assessment methods that complement each other. That includes written exams, practical assessments such as OSCE (Objective Structured Clinical Examination), assessment of communicative skills and personal reflection through portfolios. Each of these tools has the potential to capture different facets of medical competence, providing a more complete picture of student development.
You written exams, including multiple choice questions and essays, are effective in assessing theoretical knowledge and conceptual understanding. However, to measure the applicability of this knowledge in real situations, methods such as OSCE are indispensable. These simulate real clinical scenarios where students must demonstrate their practical skills, from diagnosis to proposing a treatment plan.
The assessment of communication skills is another fundamental pillar. Methods like 360-degree assessments and feedback from simulated patients offer valuable insights into students' ability to communicate effectively with patients, families, and the healthcare team. This skill is crucial, as effective communication is intrinsically linked to patient safety and quality of care.
O portfolio, on the other hand, serves as a reflective tool, encouraging students to reflect on their learning experiences, successes, and areas for improvement. This promotes a self-directed learning and a growth mindset, preparing them for the continuous and adaptive medical practice required in the 21st century.
To successfully implement these diverse assessments, it is critical that medical education institutions invest in adequate training for assessors, ensuring that they are well-equipped to administer, observe, and evaluate assessments fairly and consistently. Furthermore, there must be a robust feedback system, where students receive constructive guidance on how they can improve, closing the learning cycle.
By adopting these approaches to assessment in a competency-based curriculum, medical schools can ensure that their graduates are not only academically prepared, but also adequately equipped with the practical, ethical, and communicative skills needed to meet the demands of patient care in the world. real.
4. Feedback and Reflection
Implementing the Competency-Based Curriculum in medical education is a transformative process that requires a comprehensive commitment to improving the quality of teaching and learning. This model emphasizes the development of essential skills that students must acquire to be effective professionals and responsive to the needs of society.
A critical step in this process is the Feedback and Reflection. Feedback, whether formal or informal, is vital to students' ongoing professional development. It offers a unique opportunity to identify areas of strength and those in need of improvement. Therefore, educational institutions must cultivate a culture where feedback is seen as a tool for growth, not criticism. This involves creating open and safe channels for the exchange of feedback between teachers and students, as well as between students themselves.
A self-evaluation, complementary to external feedback, allows students to reflect on their own learning experiences. It promotes metacognition, where students become more aware of their own learning process, identify their gaps in knowledge and skills, and develop plans to overcome them. This not only fosters independence in learning but also prepares students for continuing medical education, a requirement in medical practice.
Furthermore, effective implementation of a competency-based curriculum requires the integration of practical activities that simulate real work situations. This includes everything from simulated clinical care, such as OSCEs (Objective Structured Clinical Examinations), to research projects and community work. Such activities provide students with a solid foundation for applying theoretical knowledge in practical contexts, developing essential decision-making, teamwork and effective communication skills.
The role of teachers, tutors and preceptors is also fundamental in this model. Not only do they provide the feedback needed to develop skills, they also model the professional and ethical behavior expected of future doctors. The mentoring and preceptorship relationship helps to build a bridge between theory and practice, guiding students through real examples of how skills can be applied in patient care.
For feedback and reflection to be more effective, institutions need to adopt assessment tools that can accurately measure the student's progress in relation to the defined competencies. This may include portfolios, self-assessments, peer reviews, and more. These tools must allow the identification of progress and development needs, in order to guide personalized educational interventions.
In short, Feedback and Reflection are essential pillars in the implementation of competency-based curriculum in medical education. They not only improve the quality of learning, but also prepare students for a medical career that is responsive and adaptive to the changing health needs of the population.
As we explore the characteristics of a competency-based curriculum, it is critical to also consider the implementation challenges and strategies. In the next section, we will delve into the complexities of adapting traditional curricula to this innovative model, discussing the barriers faced by educational institutions and potential solutions to overcome them.
Challenges and Opportunities
While transitioning to a competency-based curriculum presents challenges, including the need for significant cultural changes and engagement of all stakeholders, the opportunities are vast. This approach promotes more relevant and adaptive medical education, preparing physicians not only for current challenges but also to be agents of change in promoting better health.
The shift to a competency-based curriculum in medical education reflects a necessary evolution to meet the expectations of a society that demands a high level of professionalism, skill and compassion from its doctors. By focusing on developing comprehensive professional competencies, we are redefining medical education to better meet the needs of patients and meet the challenges of an ever-changing healthcare environment. This is a time of transformation, promising not only to improve the quality of healthcare but also to enrich the educational journey of future doctors.
The implementation of a competency-based curriculum professionals in medical education brings to light a complex set of challenges and opportunities. This educational model, which focuses on developing the skills, knowledge and attitudes necessary for medical practice, represents a significant evolution in the way future doctors are trained. Addressing these challenges requires substantial cultural change within educational institutions, as well as ongoing commitment from all stakeholders, including educators, students, and the healthcare system as a whole.
Challenges to be Overcome
One of the main challenges in adopting a competency-based curriculum is the need to cultural change in educational institutions. Traditionally, medical curricula have been structured around contact hours and syllabus, rather than skills to be acquired. The transition to a student-centered model demands a complete review of the teaching-learning methodology, requiring that educators be trained to adopt new pedagogical practices focused on active teaching-learning and formative assessment methodologies.
Another significant challenge is ensuring the engagement of all interested parties. This includes not only educators and students, but also regulatory bodies, hospitals and clinics that provide practical training. Collaboration between these parties is crucial to creating a learning environment that truly supports the development of professional skills.
Opportunities Provided
On the other hand, adopting a competency-based curriculum offers multiple opportunities. One of them is the training more qualified professionals, who are better prepared to meet the needs of a constantly evolving healthcare system. The emphasis on competencies allows students to apply theoretical knowledge to real-world practical situations, developing critical skills for effective medical practice.
Furthermore, this model promotes personalized education, where student progress is measured by the acquisition of skills and not by time spent in the classroom. This allows students to advance at their own pace, dedicating more time to areas that require additional attention, which can result in better-prepared and confident professionals.
Implementing a competency-based curriculum also paves the way for educational innovation. The focus on competencies encourages the use of teaching technologies, such as simulations and problem-based learning (PBL), which can enrich the learning experience and better prepare students for the challenges of medical practice.
Finally, the transition to a competency-based curriculum in medical education is an opportunity to reformulate medical training in order to align more closely with the needs of society and the healthcare system. This includes preparing physicians not only as care providers, but also as leaders, researchers, and public health advocates.
In short, while the challenges are significant, the opportunities offered by a professional skills-based curriculum are transformative. Overcoming these challenges requires collaborative effort, creativity, and a commitment to continuous improvement in medical education. As we move on to the next section, we will explore how institutions can effectively navigate this transition, highlighting strategies and best practices for successfully implementing competency-based curricula in medical education.
Conclusion
The movement towards a competency-oriented medical curriculum represents a milestone in medical education, with the potential to train more qualified, adaptable and humanized professionals. This approach ensures that future doctors are ready to face not only the technical, but also the ethical and humanistic challenges of medical practice.
How to Make the Transition?
The transition to a competency-based medical curriculum marks a significant turning point in medical education. This revolutionary approach aims to train healthcare professionals who are not only technically proficient, but also adaptable, empathetic and fully prepared to face the complex challenges of today's healthcare scenario. This movement represents an essential evolution in the way we educate future doctors, ensuring that they are equipped not only with the knowledge, but with the skills and attitudes necessary for excellent medical practice.
Implementing a competency-based curriculum offers a series of undeniable benefits. It promotes more relevant and adaptive medical education, preparing doctors for the contemporary challenges of medicine, including technical, ethical and humanistic aspects. The focus on competencies ensures that students develop a deep and applicable understanding of their field, as well as essential skills such as effective communication, critical thinking, and ethical decision-making.
This educational model emphasizes the importance of continuous learning and adaptation to new technologies and information, essential characteristics for any healthcare professional in the 21st century. By focusing teaching on skills, medical curricula facilitate students' transition from the classroom to real clinical environments, promoting smoother and more effective integration into the healthcare system.
Furthermore, the competency-driven curriculum has the potential to significantly improve patient care. By focusing on developing practical skills and applying knowledge in real-life scenarios, future physicians are better prepared to meet patients' needs in a compassionate and efficient manner, contributing to a more positive healthcare experience and health outcomes. best.
However, implementing this model is not without challenges. Requires significant cultural changes within educational institutions, as well as the commitment and collaboration of everyone involved in the educational process. The necessity of adequate resources, faculty training, and innovative assessments are critical aspects for the success of this transition.
In view of the challenges and opportunities presented, it is clear that a competency-based curriculum is the way forward in medical education. It represents a commitment to excellence in the training of doctors, ensuring that they are ready to contribute significantly to the health and well-being of the population.
Common questions
A professional competence is an integrated combination of knowledge, skills, attitudes and values that allow an individual to effectively carry out the activities of their profession in different contexts. In the context of medicine, this implies not only the ability to apply scientific and technical knowledge to the diagnosis and treatment of diseases, but also the ability to communicate effectively with patients and colleagues, make ethical decisions under pressure, work as a team multidisciplinary and adapt to new technologies and procedures.
Professional skills are developed through a continuous process of learning and practice, aiming for excellence in patient care and continuous improvement in the quality of health services. A medical curriculum based on professional competencies is structured to ensure that all medical students acquire these essential competencies throughout their training, through active teaching-learning methodologies, formative assessments and supervised clinical experiences.
This educational model emphasizes the practical application of knowledge, solving real problems, reflection on practice, and ongoing personal and professional development. By focusing on professional competencies, the medical curriculum prepares future doctors not only to respond to the challenges of current medical practice, but also to be agents of change, capable of contributing to the evolution of medicine and the promotion of health in their communities.
Competence is the ability to mobilize and apply a set of knowledge, skills, attitudes and values in an integrated manner to efficiently carry out specific activities in varied contexts. In the context of medical education, skills are not limited to technical knowledge; they encompass the ability to use this knowledge in a practical, ethical and effective way in decision-making, communicating with patients and teams, and managing complex health situations.
For example, in medical practice, a core competency is "effective communication." This involves not only the ability to explain medical conditions and treatments in a clear and understandable way to patients, but also active listening skills, empathy, and the ability to adapt communication to different cultural and emotional contexts. Another core competency is "evidence-based decision making," which requires skills to seek, evaluate, and apply the best available scientific evidence, along with clinical judgment and patient preferences, to make decisions about care.
Additionally, "interprofessional collaboration" is a crucial competency, involving the ability to work effectively and respectfully with a multidisciplinary healthcare team, promoting a collaborative environment that maximizes patient outcomes. These examples illustrate how competencies combine different aspects of medical practice, emphasizing the importance of a holistic approach to medical training that prepares future doctors for the challenges of contemporary practice.
Describing professional competence involves articulating specific skills, knowledge, attitudes and values that an individual must possess and demonstrate to perform tasks and functions effectively within a profession. In the context of a medical curriculum based on professional competencies, this means clearly defining the capabilities that medical students must acquire to respond to the demands of modern medical practice. A professional competency description details not only what the professional is capable of doing, but also how and why tasks are performed in a certain way.
For example, a professional competency in medicine might be "effective patient health management", which includes the ability to diagnose and treat medical conditions, but also encompasses effective communication with the patient and family, coordination of care with other professionals healthcare, and the use of resources in an ethical and efficient manner. To describe this competency, it is necessary to specify the underlying medical knowledge, clinical and communication skills, attitudes of empathy and professionalism, and the values of integrity and respect for patient autonomy.
Furthermore, it is important that the description of professional competence is accompanied by clear assessment criteria, which allow both educators and students to measure progress in the development of these competences. This may include practical assessments such as direct observation of procedures, simulation assessments, reflective portfolios, and 360-degree feedback from colleagues, patients, and supervisors. Thus, describing professional competence in the competency-based medical curriculum involves an integrated approach that combines theory and practice, focused on preparing students for the real challenges of the medical profession.
Developing a medical curriculum based on professional competencies is a complex task that requires careful planning and a systematic approach. The first step involves clearly defining the competencies that medical students need to develop to become effective and responsible professionals. This is done through collaboration between medical educators, healthcare professionals, patient representatives and other stakeholders, ensuring that the curriculum is aligned with societal needs and professional standards.
After defining the skills, the next step is to structure the curriculum in a way that promotes the development of these skills throughout medical training. This implies the integration of active learning methodologies, such as Problem-Based Learning (PBL), Project-Based Learning (PjBL), clinical simulations and practical internships, which allow students to apply knowledge in real contexts and develop practical skills, decision making and communication. Furthermore, it is essential to incorporate moments of reflection and self-evaluation, encouraging students to take responsibility for their own learning and professional development.
Finally, student assessment must be carried out in a continuous and formative manner, using a variety of instruments that allow assessing not only theoretical knowledge, but also practical skills, attitudes and values. This includes practical assessments, 360-degree feedback, reflective portfolios, among other methods. The curriculum must be flexible and capable of adapting to changes in medical practices and the needs of society, ensuring medical training that prepares future professionals for the challenges of contemporary medicine.
See in this article how to structure a resume by competency in medicine
When developing a medical curriculum based on professional skills, it is crucial to specify the skills that distinguish the training offered, reflecting students' preparation to face the challenges of medical practice effectively and responsibly. In the curriculum, the competencies divided into categories must be detailed, such as clinical, professional, communicational, and ethical competencies, describing not only what the student should know, but also what they should be able to do and how they should behave in different professional contexts.
For example, clinical skills may include the ability to make accurate diagnoses, develop effective treatment plans, and perform technical procedures safely. In professional skills, the importance of continuous learning, interdisciplinary teamwork and leadership is emphasized. Communication skills encompass the ability to communicate clearly and empathetically with patients, family members and teammates. And, finally, ethical competencies involve decision-making based on ethical and legal principles, respecting patient autonomy and promoting justice in health care. You can also use the competency structure of the National Curricular Guidelines (DCNs) for Medicine.
Furthermore, it is important to include teaching and assessment methods that support the development of these skills, such as simulations, practical internships, portfolio-based assessment and 360-degree feedback. This detail in the curriculum demonstrates a commitment to a medical education that prepares students not just technically, but as well-rounded professionals capable of contributing significantly to the health and well-being of patients in an ever-evolving healthcare environment.
A competency-based structured medical curriculum is designed to ensure that medical students acquire not only the necessary theoretical knowledge, but also the practical skills, attitudes and values essential for medical practice. This approach is adopted when educational institutions recognize the need to prepare healthcare professionals who are capable of responding effectively to the challenges and demands of the contemporary healthcare system. The transition to a competency-based curriculum reflects a commitment to education that is relevant, integrated, and results-oriented in clinical practice.
The structuring of the curriculum with a focus on skills takes place in a context where medical training seeks to align itself more closely with the needs of patients and society. This entails a shift from a traditional teacher- and content-centered model to a student-centered model of active learning and ongoing professional development. Skills such as effective communication, critical thinking, interprofessional teamwork and the ability to learn autonomously become as important as mastering medical knowledge.
To implement this model, educational institutions adopt pedagogical strategies, such as problem-based learning (PBL), project-based learning (PjBL), clinical simulations and supervised practical internships, which promote the application of knowledge in real contexts. Assessment is also restructured to focus on demonstrating competencies through methods such as direct observation, reflective portfolios and 360-degree assessments. This approach ensures that, upon completing training, future doctors are prepared to provide high-quality care, guided by an ethical commitment and evidence-based practice.
To create an effective, professional competency-based medical curriculum, it is crucial to identify and integrate a comprehensive set of competencies that medical students must acquire to meet the demands of contemporary medical practice. These competencies must be explicitly described in the curriculum to guide both the learning process and assessment. Here are essential elements to include:
1. Clinical and Technical Skills: Detail the skills necessary for diagnosing and treating patients. This includes taking detailed histories, performing competent physical examinations, interpreting laboratory and imaging tests, safely performing basic and emergency procedures, and developing evidence-based therapeutic plans. The ability to integrate medical knowledge to facilitate clinical decision making should be a key competency described.
2. Interpersonal and Communication Skills: Emphasize the importance of effective communication with patients, families and the healthcare team. Include skills such as the ability to establish an empathetic therapeutic relationship, communicate diagnoses and treatment plans in a clear and accessible way, and work effectively as a team. The ability to listen actively, negotiate care plans, and manage conflict constructively are also essential skills.
3. Professional, Ethical and Reflective Skills: Point to the need for ethical practices in decision-making, respecting the rights and dignity of patients. Highlight the importance of self-assessment and continuous learning, including the ability to critically reflect on one's practice, recognize limitations, and seek additional knowledge and skills. Adherence to the principles of bioethics, the commitment to continuous improvement in the quality of care and public health, as well as the effective management of health resources, are competencies that must be clearly articulated.
Furthermore, with the growing importance of technology in medicine, digital health skills, such as the effective use of health information systems and the application of emerging technologies in patient care, must also be included. By detailing these skills in the curriculum, medical education institutions establish a clear roadmap for students' professional development, ensuring that they are prepared for the challenges of modern medical practice.
In the competence-based education proposal, the curriculum is defined as a structured set of skills that students must develop to become efficient, ethical professionals and responsive to the needs of society. This educational model emphasizes learning oriented towards the practical application of knowledge, skills, attitudes and values in real contexts of medical practice. Defining the curriculum begins with identifying the essential competencies required by healthcare professionals, including technical capabilities, communication skills, critical thinking, problem solving and professionalism.
To structure the curriculum in a competency-based education proposal, it is necessary to map the teaching, learning and assessment activities that promote the development of these competencies. This entails the integration of active pedagogical methods, such as case studies, simulations, problem-based learning (PBL), project-based learning (PjBL) and clinical internships, which allow students to experience and reflect on medical practice in a controlled environment and supervised. The curriculum must be flexible and adaptable, allowing customization to meet individual student needs while ensuring the acquisition of essential skills.
Furthermore, competency-based curriculum requires an assessment system that measures students' progress toward defined competencies. Assessments must be formative, providing regular and development-oriented feedback, as well as summative, to certify the acquisition of skills at the end of the educational process. This model curriculum highlights the importance of continuous learning and self-assessment, preparing students for a career of perpetual learning and adapting to changes in medicine and the health needs of the population.
In a resume focused on professional skills, it is essential to highlight skills, knowledge and attitudes that demonstrate your ability to perform effectively in the medical field. To this end, priority must be given to the inclusion of skills that reflect practical experiences, academic training and personal development.
First, include technical skills acquired through your training and professional experience. This encompasses knowledge in specific areas of medicine, skills in clinical procedures, diagnosis and treatment of diseases, as well as the application of evidence-based practices.
Next, highlight interpersonal and communication skills, crucial for effective interaction with patients, family members and multidisciplinary teams. This includes empathy, active listening skills, the ability to convey complex information in a clear and understandable way, and working collaboratively.
Last but not least, mention skills related to ethics and professionalism, such as integrity, responsibility, commitment to continuous learning and adaptation to dynamic work environments. Furthermore, health management and leadership skills can be a differentiator, reflecting your ability to contribute to the improvement of health systems and the well-being of the community. By compiling these competencies on your resume, you offer a holistic view of your capabilities and preparedness to face the challenges of modern medicine.
When talking about competencies in the context of a medical curriculum based on professional competencies, it is crucial to adopt a holistic approach that encompasses not only the technical aspects of medicine, but also the interpersonal, ethical and professional skills necessary for effective and humanized medical practice. Start the discussion by clearly defining what competencies are - the integration of knowledge, skills, attitudes and values that enable doctors to perform their roles efficiently in different contexts.
A fundamental step is to identify and describe the specific competencies required in contemporary medicine, such as diagnosis and clinical management, effective communication with patients and teams, ethical decision-making, continuous learning, and the ability to adapt to new technologies and practices. These competencies must be aligned with patient needs and healthcare system challenges, ensuring that clinicians are prepared to provide high-quality, patient-centered care.
When talking about how these skills are developed and evaluated within the medical curriculum, it is important to highlight the use of active teaching methodologies and simulation-based practices, supervised clinical internships and research projects that allow students to apply and improve their skills in real contexts. . Competency assessment should be ongoing and multifaceted, using tools such as 360-degree feedback, reflective portfolios and direct observation to measure not only technical knowledge, but also communication skills, clinical reasoning and professionalism. Discussing competencies in this way highlights the importance of medical training that is in tune with the demands of the 21st century, preparing doctors not only to cure, but to provide compassionate and competent care.
An integrated curriculum and a competency-based curriculum represent two distinct educational approaches, both with the aim of optimizing the learning process, but with different focuses and strategies.
The integrated curriculum is characterized by the connection and interdisciplinarity between the different areas of knowledge. In this approach, subjects are not taught in isolation, but integrated in order to provide students with a more holistic and applied understanding of knowledge. The focus is on how concepts and skills from different disciplines relate and can be applied in real contexts, promoting more meaningful learning. This integration can occur between disciplines within the same field, such as different areas of medicine, or between different fields, such as medicine, ethics and social sciences, aiming to prepare the student for the complex challenges of professional practice.
On the other hand, a competency-based curriculum emphasizes the development of specific skills, knowledge, attitudes and behaviors that students need to acquire to become competent professionals. In this model, student progress is assessed based on demonstration of predetermined skills, not just course completion or content memorization. This type of curriculum focuses on "knowing how to do" in practical situations, preparing students to apply what they have learned effectively in the workplace. Learning is often self-directed, with students taking responsibility for their own development, guided by clear learning goals and ongoing assessment.
While the integrated curriculum seeks to offer a more connected and applied view of knowledge, the competency-based curriculum focuses on ensuring that students acquire the skills and attitudes necessary for professional practice. Both models represent efforts to make education more relevant and adapted to the needs of students and society, and can be complementary when implemented strategically to enrich the educational experience.
When designing a medical resume focused on skills and competencies, it is important to highlight both technical capabilities specific to medical practice and essential interpersonal and professional skills. Initially, fundamental clinical skills should be included, such as accurate diagnosis, ability to manage treatments, perform specific procedures safely, and an evidence-based approach to clinical decision-making. These skills demonstrate the doctor's ability to effectively care for patients, using technical and practical knowledge.
Furthermore, interpersonal skills are crucial to effective medical practice and should be highlighted. This includes the ability to communicate clearly and effectively with patients, families and other members of the healthcare team, active listening skills, empathy and the ability to build therapeutic relationships. Skills in teamwork, leadership, and conflict management are also important, reflecting the ability to collaborate within interdisciplinary teams to provide integrated patient care.
Finally, one should not forget to mention competencies related to medical professionalism, which include medical ethics, commitment to continuous improvement in the quality of care, self-management and continuous professional development, and adaptation to changes in the healthcare environment. Including skills related to health information technology, such as competence in using electronic medical records and telemedicine, reflects adaptation to current trends in medical practice. This comprehensive set of skills and competencies highlights a professional prepared to face the challenges of modern medicine, committed to excellence in patient care and the continuous development of their professional capabilities.
Competency Pedagogy is an educational approach that prioritizes the development of integrated competencies — knowledge, skills, attitudes and values — necessary for students to act effectively in diverse professional and social contexts. This teaching methodology moves away from the traditional model, centered on the transmission of content, to emphasize the practical application of knowledge, encouraging active learning, real problem solving and evidence-based decision making. In the context of medical education, this means preparing students not only with in-depth theoretical knowledge, but also with the clinical, ethical, and communication skills necessary for compassionate and competent medical practice.
This approach requires significant curricular restructuring, where subjects are organized in a way that promotes interdisciplinarity and integration of knowledge. Assessment also changes, focusing less on standardized memorization tests and more on formative assessments that measure the student's ability to apply knowledge in practical situations. This involves the use of simulations, research projects, clinical internships, and other forms of practical assessment that reflect real-world competencies needed in medical practice.
Implementing Competency Pedagogy in the medical curriculum favors the development of adaptable, critical and reflective professionals, capable of continually learning and responding to rapid changes in the health field. This pedagogical model emphasizes the importance of self-assessment and continuous feedback, encouraging students to take responsibility for their own learning and professional development. In this way, Competency Pedagogy contributes to training doctors who are more prepared to face the complex challenges of contemporary medicine, improving the quality of patient care and meeting the demands of society.
Your message is important to us
Important
This is an open invitation to educators, students and healthcare professionals to engage in this educational transformation. Your participation, whether sharing experiences, ideas or challenges, is crucial to shaping the future of medical education. We are at an inflection point: together, we can lead the change toward medical education that truly meets society's needs. Are you ready to be part of this evolution?

Partner at Instituto Educater, university professor in medical courses.
He specializes in education for the health professions and writes about curricula, teacher training and artificial intelligence.